Individuals with stage A should be treated with therapies that can delay progression of cardiac dysfunction and development of heart failure.
Optimizing hypertension treatment based on the current (JNC VII) can reduce new-onset heart failure by 50%. Therapies such as diuretics, β-blockers, angiotensin-converting enzyme inhibitors (ACEIs), and angiotensin II receptor blockers (ARBs) are proven to be more effective than calcium channel blockers and doxazosin in preventing heart failure.
Use of statin therapy in CAD patients based on current hyperlipidemia guidelines [ATP III] can also reduce the incidence of heart failure by 20%.
Evidence-based disease management strategies for atherosclerotic vascular disease, and thyroid disease, as well as patient avoidance of tobacco, alcohol, cocaine, amphetamines, and other illicit drugs that can be cardiotoxic, are also important components of early risk modification for prevention of heart failure.
In diabetic patients, both ACEIs and ARBs (specifically losartan and irbesartan) have been shown to reduce new-onset heart failure compared with placebo.
In CAD or atherosclerotic vascular disease patients without heart failure, reviews of the EUROPA and HOPE Trials results show a 23% reduction in heart failure with ACEI therapy as well as reduced mortality, MIs, and cardiac arrest.
What is treatment of systolic heart failure stage B?
Patients who do not have clinical symptoms of heart failure but who have a structurally abnormal heart, such as a previous MI, evidence of left ventricular remodeling (left ventricular hypertrophy or low ejection fraction), or valvular disease, are at a substantial risk of developing symptomatic heart failure.
Prevention of further progression in these at-risk patients is the goal, and appropriate therapies are dependent on the patient's cardiac condition
In all patients with a recent or remote history of MI, regardless of ejection fraction, ACEIs and β-blockers are the mainstay of therapy. Both therapies have been demonstrated in randomized control trials to cause a significant reduction in cardiovascular death and heart failure.
There is no clear evidence for use of ARBs in asymptomatic patients with reduced left ventricular ejection fraction; however, ARB therapy is a reasonable alternative in ACEI-intolerant patients.
What is standard treatment of symptomatic systolic heart failure (stage c)?
The overall goals in this stage are to improve the patient's symptoms, slow or reverse the deterioration of cardiac functioning, and reduce the patient's long-term morbidity and mortality.
Accurate assessment of the cause and severity of heart failure, the incorporation of previous stage A and B treatment recommendations, and correction of any cardiovascular, systemic, and behavioral factors are important to achieve control in patients with symptomatic heart failure.
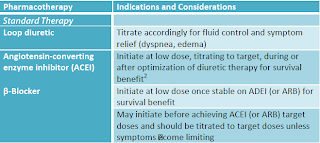
Patients with symptomatic heart failure should be routinely managed with a standard therapy of a diuretic, an ACEI (or ARB if intolerant), and a β-blocker. The addition of other pharmacologic therapies should be guided by the need for further symptom control versus the desire to enhance survival and long-term prognosis. A stepwise approach to therapy is presented in next table and expanded upon below.



No comments:
Post a Comment